SUDDEN RISE OF AUTOIMMUNE DISEASES WORLDWIDE WITH 4 OUT OF 5 CASES OBSERVED IN WOMAN
What Is an Autoimmune Disease?
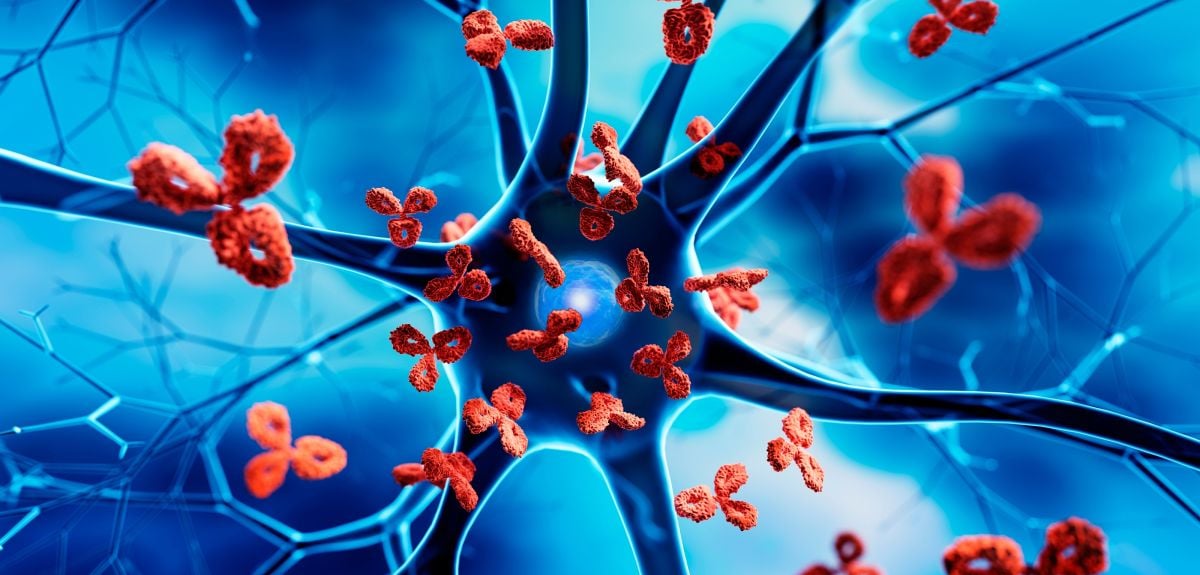
An autoimmune disease is a condition in which the immune system, which normally protects us against infections, mistakenly attacks healthy cells, tissues, or organs. Instead of defending the body, it launches a misdirected response, leading to inflammation, damage, and chronic illness.
There are more than 80 recognized autoimmune disorders, spanning a wide range of systems — from rheumatoid arthritis (joints), type 1 diabetes (pancreas), and multiple sclerosis (nervous system), to lupus, psoriasis, thyroiditis, and many others.
According to epidemiological estimates, autoimmune diseases affect around 4–5% of the population, with a significantly higher burden in women (approximately 6.4% in females vs 2.7% in males).
Why Do Autoimmune Diseases Happen?
The exact causes vary depending on the disease, but the underlying mechanisms often involve:
- Genetic predisposition: Certain gene patterns (e.g., HLA types) make people more likely to develop autoimmunity.
- Environmental triggers: Infections, toxins, and even components of the microbiome can trigger immune misfires.
- Molecular mimicry: Some pathogens bear proteins that resemble human proteins; when the immune system attacks the invader, it may also target similar “self” proteins.
- Hormonal influences: Women are disproportionately affected, and hormones (like estrogen) may play a role.
- Immune regulatory failure: The immune system has checks and balances (e.g., regulatory T cells) to prevent self-attack. When these fail, autoimmunity can arise.
Key Players: Autoantibodies and Immune Cells
- Autoantibodies: These are antibodies (immune proteins) that target “self” molecules. Rather than being bystanders, they can be direct mediators of disease.
- B-cells & T-cells: B-cells produce antibodies, while T-cells (especially certain “rogue” T-cells) can directly attack tissue.
- Complement system and immune complexes: Some autoantibodies trigger a cascade (the complement system) that damages tissue; others form immune complexes that deposit in organs.
Symptoms and Clinical Presentation
Autoimmune diseases can be highly variable, because they can target almost any part of the body. Common themes include:
- Chronic inflammation (pain, swelling, redness)
- Fatigue
- Organ-specific symptoms (e.g., joint stiffness in rheumatoid arthritis, numbness or weakness in multiple sclerosis)
- Periods of flares (worsening) and remissions
Because symptoms overlap with many other conditions, diagnosis can be challenging and slow.
Advances in Diagnosis (2025)
Diagnosis of autoimmune disease is improving, thanks to molecular and technological advances:
- Molecular diagnostics: Researchers are developing tests that identify disease-causing “rogue” immune cells (B- and T-cells) by tracking their unique receptors (“barcodes”).
- AI and Machine Learning: Artificial intelligence is increasingly used to analyze clinical and molecular data to predict disease onset, flare-ups, or treatment responses.
- Proteomic biomarkers: For example, in systemic lupus erythematosus (SLE), proteomics (large-scale protein analysis) is being used to identify proteins that predict flare risk in certain populations.
- Autoantibody testing: Sophisticated assays are being refined, not only to detect autoantibodies but also to understand their role in disease (pathogenic vs benign).
Current Treatments: Traditional & Emerging
Historically, autoimmune diseases have been treated with broad immunosuppression: steroids, disease-modifying anti-rheumatic drugs (DMARDs), biologics. While effective, these therapies suppress the immune system broadly and come with side-effects (infection risk, long-term toxicity).
Emerging & Next-Generation Therapies
Recent years have seen a paradigm shift: instead of just suppressing the immune system, scientists are working to reprogram or reset it.
- CAR-T therapy: Originally developed for cancer, CAR-T (chimeric antigen receptor T-cell) therapy is being repurposed to eliminate autoreactive B-cells.
- Bispecific antibodies & cytokine modulation: New immunotherapeutics are being developed to more precisely regulate immune signaling.
- Stem cell therapy: Clinical trials around the world are exploring stem-cell-based treatments to modulate immunity and repair tissue.
- Gene-editing / CRISPR: Experimental work aims to correct genetic drivers of autoimmunity.
- Microbiome interventions: Because gut bacteria influence the immune system, therapies targeting the microbiome are under investigation.
Emerging Challenges
- Safety and long-term effects: Precision therapies like CAR-T are promising, but long-term safety (especially in non-cancer settings) needs careful evaluation.
- Cost and access: These advanced therapies are expensive, and not readily available everywhere.
- Regulatory hurdles: New modalities (gene editing, cell therapy) require rigorous regulatory frameworks.
- Early diagnosis: Because autoimmunity often begins long before symptoms, early detection is a challenge.
- Research funding: According to recent reports, funding cuts threaten the pace of autoimmune therapy development.
Special Considerations: Gender & Autoimmune Risk
- As mentioned, women make up nearly 70% of autoimmune disease patients.
- Hormonal fluctuations (e.g., pregnancy, menopause) and genetic factors (e.g., X-chromosome biology) may contribute to this disparity.
- Underdiagnosis in women is a concern, especially because many autoimmune symptoms (fatigue, pain) are non-specific.
Recent High-Impact Developments
- IgG4-Related Disease Treatment: In April 2025, the U.S. FDA approved inebilizumab (Uplizna) for IgG4-related disease, marking a milestone as the first therapy for this rare but serious immune disorder.
- Coeliac Disease Diagnosis: Researchers in Australia have developed a blood test that detects immune markers (IL-2, gluten-specific T-cells) to diagnose celiac disease without requiring gluten exposure.
- CAR-T / Immune Resetting: There is growing momentum toward using CAR-T and related immune-resetting therapies for conditions like lupus, rheumatoid arthritis, and multiple sclerosis.
- Vitamin D Study in MS: A French study (published in JAMA) suggests that high-dose vitamin D3 (100,000 IU biweekly) in early multiple sclerosis may reduce disease activity.
The Road Ahead: Future Directions & Hope
- Precision medicine: Tailoring immunotherapies to the individual (using molecular diagnostics, AI, and biomarkers) is likely to become the norm.
- Immune tolerance induction: Instead of blanket suppression, the goal is to teach the immune system to tolerate self — via approaches like “inverse vaccines” or antigen-specific therapies.
- Regenerative therapies: Stem cells + tissue-repair strategies may not just halt disease but help heal damage.
- Prevention: Identifying people at risk (via genetics, early biomarkers) may allow preventive therapies before full-blown disease develops.
- Global access: For these breakthroughs to make a real-world impact, cost, infrastructure, and equitable access are critical.
Key Takeaways for Patients & Caregivers
- Autoimmune diseases are complex and diverse, but progress in diagnostics and therapy is accelerating.
- If you have persistent symptoms (fatigue, joint pain, unexplained inflammation), advocating for a specialist evaluation (e.g., rheumatologist, immunologist) can be important.
- Precision therapies may become increasingly available, but they also come with higher costs and potential risks — shared decision-making is essential.
- Lifestyle factors (diet, stress management, sleep) remain important — while they may not cure autoimmune disease, they can support overall immune health and complement medical treatment.
- Stay informed: Research is rapidly evolving, and clinical trials may offer access to cutting-edge therapies.
Conclusion
Autoimmune diseases pose a significant and growing challenge for global health. But as of late 2025, we are witnessing a transformative moment: a shift from broad suppression toward precision, resetting, and potentially curative approaches. Advances in immunotherapy, AI-driven diagnostics, and molecular medicine are converging to give new hope to patients who have long relied on symptom control. While challenges remain—especially regarding access, long-term safety, and early detection—the future is increasingly optimistic.
-------Author: Team Saistho.
--------------------------------------